Specialist in:
Knee Surgery;
Orthopedics and Traumatology;
Sports Medicine.
Contact
+55 (11) 2151-5317
Knee
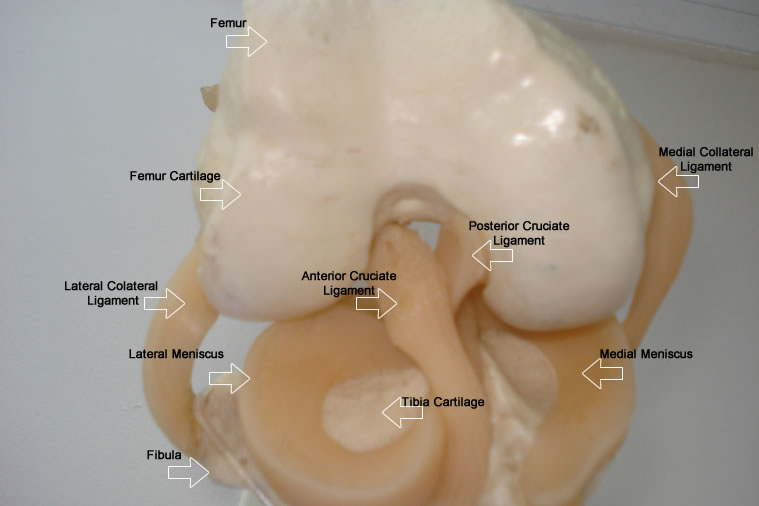
What is the knee?
The knee is a joint that is formed by the bone extremities of the thigh (femur), the leg (tibia and fibula) and the patella (kneecap). The ligaments, tendons, menisci and muscles are also elements of the knee structure.
Click to see a video demo
What is the function of the knee structures?
The bone surfaces are covered with cartilage (substance similar to hardened gelatin) and assist on dampening.
Dampening is supported by menisci, which are also responsible for providing more stability to the knee. The menisci have similar consistency to the cartilage and are located above the leg cartilage at the level of the knee. We have two menisci, medial – on the inside of the knee – and the lateral one – outside the knee.
The anterior and posterior cruciate ligaments and the medial and lateral collateral ligaments are structures similar to fibrous cords that connect the thighbone to the leg bone in order to provide stability (firmness) to the knee.
There are several muscles to provide movement to the knee. In particular, the quadriceps muscle (anterior thigh muscle) that connects to the quadricipital tendon. In turn, the kneecap is connected to the leg due to a patellar ligament to extend the leg.
What is knee osteoarthritis (degenerative joint disease)?
The osteoarthritis is a cartilage erosion that exposes the bone. Pain while moving the knee is mainly caused by friction on the exposed bone (without cartilage coverage).
This weariness can be naturally caused throughout the years or by other causes, like rheumatoid arthritis and gout.
Trauma can affect the knee structure and lead to an early weariness of this articulation.
Click to see a video demo
Is conservative (non-surgical) treatment possible to knee arthritis?
Knee conservative treatment should be individualized to each patient and it involves the use of:
- Painkillers and Anti-inflammatory drugs,
- Medication to delay weariness worsening and take the pain away [chondro-protectors (glucosamine sulfate and diacerein) and the infiltration (viscosupplementation - hyaluronic acid)],
- Loss of weight,
- Use of crutches,
- Use of insoles,
- Physiotherapy,
- Acupuncture.
Should I strengthen my knees with osteoarthritis or should I stop with physical activity?
The strengthening of knees with osteoarthritis should be encouraged taking into account the limits of each individual. Besides, perform stretching exercises for the muscles, which are normally shortened and stiffened.
Should I use hot or cold packs for knee osteoarthritis?
The best studies show that both are beneficial, but patients who use the cold pack tend to need fewer painkillers.
The cold pack in addition to having analgesic effect reduces the installation of the inflammatory process.
The hot pack also features analgesic effect, promotes the drainage of the inflammatory process and relaxes the muscles that are usually stiffened.
How is the surgical treatment for total knee osteoarthritis?
On the failure of treatment without surgery and when the pain becomes difficult to control and disturbs the quality of life of the individual, prosthesis (total arthroplasty) of the knee is indicated.
In this surgery, the exposed bone part with worn out cartilage is removed.
Then, the exposed bones are covered by a new metallic coverage (similar to the shape of the original knee surfaces).
A component made from special plastic is placed between the metal surfaces.
This procedure removes the friction between the exposed bones providing analgesic effect.
The patient resumes movements on the same day of surgery and begins to walk on the second day with the aid of a walker..
Click to see a video demo
Click to see a video demo
Click to see a video demo
Click to see a video demo
Click to see a video demo
Click to see a demo image
Click to see a video demo
How is the surgical treatment for partial knee osteoarthritis for older patients?
In cases of older patients with localized wear and no major misalignment on the knee, more localized and economic bone cutting through the unicompartmental (tibiofemoral or patellofemoral) knee prosthesis is an option.
Click to see a video demo
How is the surgical treatment for partial osteoarthritis of misaligned knee on a younger patient?
Misalignment of the knee [inward (genu valgum) or outward (genu varum) knees] can cause located overload in an area with greater contact with the knee, as a misaligned car tire that gets more worn where there is more contact.
In the case of younger and/or active patients, the alignment of the knee should be performed through osteotomy.
This procedure is a cutting to the bone to allow correction of alignment.
This alignment is maintained due to a plate and screws that can be removed after consolidation of the bone cutting.
Click to see a video demo
What's new to improve knee surgery precision?
Computerized navigation can be used to support accuracy of alignment of the prosthesis and osteotomy.
Older people should not perform surgery for knee osteoarthritis?
With medical advances, life expectancy of the population increases.
And although osteoarticular diseases do not lead to death, they cause disabling pain, taking the individual away from their social life and can even cause depression and anxiety.
The greatest need of surgery due to worn out knee is exactly for this age group.
Therefore, surgery should be provided as safe as possible through a preoperative evaluation including blood tests, cardiology exams and control of other existing diseases.
Is there risk-free surgery? What can be done to provide safer surgery?
Unfortunately, there is no risk-free surgery.
However, a cautious, careful and updated surgeon knows the risks and possible ways to minimize them through a pre-operative evaluation.
The postoperative care involves antibiotics to prevent infection and measures to prevent thrombosis, when necessary.
What to do to avoid deep vein thrombosis after a surgery for knee osteoarthritis?
Patients who underwent total knee replacement should perform thrombosis prevention (blood clot in blood vessels) by gait and early motion, wearing elastic stockings, use of medication to prevent thrombosis and the use of an intermittent pneumatic compression device.
What is osteochondritis?
Osteochondritis dissecans is a disease with detachment of the cartilage and bone.
This fragment can detach itself from the knee.
This injury can occur with or without trauma and often affects younger patients. If there is detachment of the fragment, conservative treatment is indicated, unlike the situation of detached fragment.
How can cartilage initial and located lesions be treated after trauma?
For these lesions, mosaicplasty, ice-picking, osteochondral transplantation and autologous chondrocyte transplantation can be performed to provide new cartilage as similar as possible to the original one.
What is chondromalacia patella?
Chondromalacia is the lesion to the cartilage of the kneecap, often caused by overload, poor alignment or changes in the shape of the knee (patellofemoral syndrome) and trauma.
Some cases may be idiopathic (unknown cause).
Initially, treatment is conservative, but may require surgical treatment since some cases can progress to severe wear of cartilage or dislocation (patella is displaced from its normal position).
In the future, what are the possible treatments for cartilage lesions?
The studies are focused on stem cells, gene therapy, growth factors and nanotechnology, among others.
What is osteonecrosis?
Osteonecrosis is bone necrosis, which can lead to the collapse of the knee surface.
The disease begins suddenly with severe pain, without obvious trauma.
The cause may be idiopathic (unknown) or by diseases such as systemic lupus erythematosus, alcoholism, Gaucher's disease, hemoglobinopathies and corticosteroids.
Depending on the characteristics, the knee can benefit from surgical treatment.
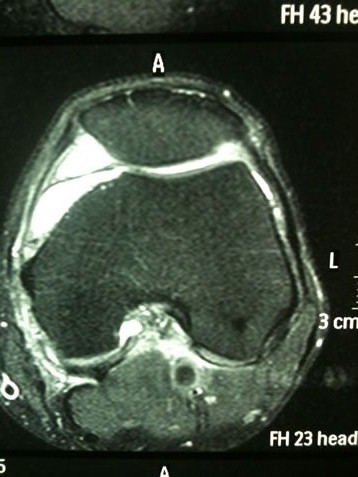
What is arthroscopy?
Arthroscopy is a method that allows treatment with a mini-camera and surgical instruments inserted into the knee through two small incisions with less than 1 cm.
These instruments have great range and allow to perform various operations to the ligaments, cartilage, meniscus and synovium.
These small arthroscopic cuts minimize post-surgical pain, facilitate the return to activities and decrease the risk of infection.
Click to see a video demo
How is the conservative treatment of anterior cruciate ligament injury of the knee?
It is possible to try conservative treatment by constantly strengthening the knee, but this is often insufficient to bring stability to the knee for physical activities, mainly to change the direction of motion.
New episodes of false steps of the knee can injure other structures of the knee (eg. other ligaments, meniscus and cartilage), reinforcing the indication of ligament reconstruction in active individuals.
How is the surgical treatment of anterior cruciate ligament injury of the knee?
In order to arthroscopically reconstruct the ligament, part of the patellar ligament or the flexor tendons of the semitendinosus and gracilis muscles are often used as a graft.
Return to work usually occurs on the first or second week, while the return to competitive sport between the 6th and 9th month.
Click to see a video demo
Scientific article authored by Dr. Gilberto Nakama and Knee Group-UNIFESP
Scientific article authored by Dr. Gilberto Nakama and Knee Group-UNIFESP
Scientific article authored by Dr. Gilberto Nakama and Knee Group-UNIFESP
How is the treatment of meniscus injury?
The degenerative meniscus injury (due to age or overload) is usually treated with non-surgical measures, while lesions due to trauma are treated with surgery.
In traumatic injury, part of the meniscus can detach and obstruct the knee, causing pain and locking.
New trauma on the injured menisci may increase the trace of the lesion and make the meniscus unrecoverable.
Depending on the characteristics of the injury, through arthroscopy, a suture (point or stitches), partial meniscectomy (removal of only the damaged and unrecoverable part), and even the meniscal transplant can be performed.
Typically, the return to work occurs within the first week after surgery.
Click to see a video demo
Click to see a video demo
How is the treatment of tendonitis and bursitis of the knee?
The most common tendonitis (inflamed tendon) is patellar, quadricipital, anserinus and iliotibial tract.
Initially it can be treated with physiotherapy, analgesics and anti-inflammatory drugs.
Some cases may require insoles, changes in sports planning and sporting gesture.
The shock wave therapy and platelet-rich plasma (platelet growth factor) are non-invasive therapeutic measures with promising results and should be given with caution, as they need a more convincing scientific evidence.
Eventually, some cases require surgery for pain relief.
What is platelet-rich plasma (PRP, platelet growth factor), and what are its possible benefits?
The PRP is obtained by preparing the patient's own blood in order to achieve a high concentration of growth factors to improve muscle and tendon healing and decrease pain and postoperative bleeding.
This technique has been used for many years in Europe.
What is Baker's Cyst?
Any internal derangement can cause inflammation with an increase of internal fluid distending the joint and forming the Baker's Cyst (analogous to a balloon).
Therefore, treatment should be directed to the cause of internal derangement.
What is synovial plica?
The synovial plica is a remnant development structure resembling a thickened membrane that causes pain when blocking the knee.
When it causes pain in the knee, it should be removed by arthroscopy.
What is Osgood-Schlatter?
This disease is characterized by pain and swelling of the bony insertion of the knee patellar ligament.
It is more common in boys aged 8 to 12 years.
One theory is that the disease is caused by a temporary reduction of blood supply.
It usually responds very well to conservative treatment, but eventually surgical treatment may be needed.
How are knee fractures treated?
Depending on the features, fractures of the knee bones (femur, tibia and patella) can be treated with or without surgery to approach and fix the bone fragments.
Currently, there are plates and screws that allow minimal cutting and high fixation strength, even for bones with osteoporosis.
It is important to remember that injury of ligaments , cartilage and meniscus can simultaneously occur in some fractures.
Do not wait to seek medical care, especially in cases of fracture (when there is communication between the fracture and the skin and contamination by microorganisms occurs) and compartment syndrome (swelling of soft parts that impairs blood circulation and cause severe pain).